What is a pleural effusion?
A pleural effusion is an excess accumulation of fluid in the pleural space around the lungs. 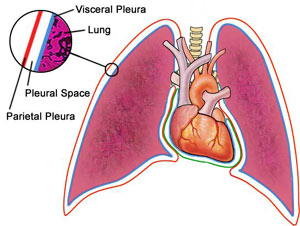 The pleura are thin membranes that enclose the lungs and line the inside of the chest cavity. The 'pleural space' describes the small space between the inner and outer layers of pleura, which normally contains a small volume of lubricating pleural fluid to allow the lungs to expand without friction. This fluid is constantly being formed through leakage of fluid from nearby capillaries and then re-absorbed by the body's lymphatic system. With a pleural effusion, some imbalance between production and reabsorption of pleural fluid leads to excess fluid building up in the pleural space.
The pleura are thin membranes that enclose the lungs and line the inside of the chest cavity. The 'pleural space' describes the small space between the inner and outer layers of pleura, which normally contains a small volume of lubricating pleural fluid to allow the lungs to expand without friction. This fluid is constantly being formed through leakage of fluid from nearby capillaries and then re-absorbed by the body's lymphatic system. With a pleural effusion, some imbalance between production and reabsorption of pleural fluid leads to excess fluid building up in the pleural space.
There are two major types of pleural effusion:
- Transudative effusions, where the excess pleural fluid is low in protein; and
- Exudative effusions, where the excess pleural fluid is high in protein
Types of fluids
Four types of fluids can accumulate in the pleural space:
- Serous fluid (hydrothorax)
- Blood ([haemothorax])
- Chyle (chylothorax)
- Pus (pyothorax or empyema)
Causes of Pleural Effusions
Anything that causes an imbalance between production and reabsorption of pleural fluid can lead to development of a pleural effusion.  Transudative pleural effusions (those low in protein) usually form as a result of excess capillary fluid leakage into the pleural space. Common causes of transudative effusions include:
Transudative pleural effusions (those low in protein) usually form as a result of excess capillary fluid leakage into the pleural space. Common causes of transudative effusions include:
- Congestive heart failure;
- Nephrotic syndrome;
- Cirrhosis of the liver;
- Pulmonary embolism; and
- Hypothyroidism.
- Pneumonia;
- Lung cancer, or other cancers;
- Connective tissue diseases, including rheumatoid arthritis and systemic lupus erythematosus;
- Pulmonary embolism;
- Asbestosis;
- Tuberculosis; and
- Radiotherapy.
Physical findings are variable and depend on the volume of the pleural effusion. Generally, there are no physical findings for effusions smaller than 300 mL. With effusions larger than 300 mL, findings may include the following:
- Dullness to percussion
- Decreased tactile fremitus
- Asymmetric chest expansion, with diminished or delayed expansion on the side of the effusion: Dullness to percussion, decreased tactile fremitus, and asymmetric chest expansion are the most reliable physical findings of pleural effusion.
- Diminished or inaudible breath sounds
- Egophony ("e" to "a" changes) at the most superior aspect of the pleural effusion
- Pleural friction rub
- Other findings that provide clues to the etiology of the effusion include the following:
- Peripheral edema, distended neck veins, and S 3 gallop, suggestive of congestive heart failure
- Edema may also be a manifestation of nephrotic syndrome; pericardial disease; or, combined with yellow nails, the yellow nail syndrome.
- Cutaneous changes with ascites, suggestive of liver disease
- Evidence of malignancy such as lymphadenopathy or palpable mass
Investigations
During a physical examination, the doctor will listen to the sound of your breathing with a stethoscope and may tap on your chest to listen for dullness.
The following tests may help to confirm a diagnosis:
- Chest x-ray

- Pleural fluid analysis (examining the fluid under a microscope to look for bacteria, amount of protein, and presence of cancerous cells)
- Thoracentesis (a sample of fluid is removed with a needle inserted between the ribs)
- Thoracic CT
- Ultrasound of the chest
Treatment
Treatment may be directed at removing the fluid, preventing it from accumulating again, or addressing the underlying cause of the fluid buildup.
Therapeutic thoracentesis may be done if the fluid collection is large and causing pressure, shortness of breath, or other breathing problems, such as low oxygen levels. Removing the fluid allows the lung to expand, making breathing easier. Treating the underlying cause of the effusion then becomes the goal.
For example, pleural effusions caused by congestive heart failure are treated with diuretics (water pills) and other medications that treat heart failure. Pleural effusions caused by infection are treated with appropriate antibiotics. In people with cancer or infections, the effusion is often treated by using a chest tube for several days to drain the fluid. Chemotherapy, radiation therapy, surgery, or instilling medication into the chest that prevents re-accumulation of fluid after drainage may be used in some cases.
During a physical examination, the doctor will listen to the sound of your breathing with a stethoscope and may tap on your chest to listen for dullness.
ReplyDeletesummer weight bedspreads
summer bedspreads king size